
Age-Related Reactions to a Traumatic Event
Describes how young children, school-age children, and adolescents react to traumatic events and offers suggestions on how parents and caregivers can help and support them.
Parents and caregivers play an essential role in helping children and teenagers recover from traumatic events. These resources are for parents, adoptive parents, resource/foster parents, grandparents, caregivers, and all others who care for children and teens. The more caregivers learn about how traumatic events affect their children (whether toddler, school-age, teen, youth, or adult), the more they understand the reasons for their children’s behaviors and emotions, and the better prepared they are to help them cope. When children know that caring adults are working to keep them safe and support them in understanding their reactions to trauma, most can recover and go on to live healthy and productive lives.

Describes how young children, school-age children, and adolescents react to traumatic events and offers suggestions on how parents and caregivers can help and support them.

Provides parents and caregivers with tools to help them support children who have been victims of sexual abuse, information on the importance of talking to children and youth about body safety, and guidance on how to respond when children disclose sexual abuse.

Defines child traumatic stress. This fact sheet gives an overview of trauma, describes traumatic stress symptoms, and ways children may be impacted.
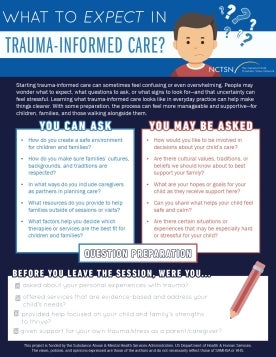
Helps families understand what trauma-informed care looks like in practice and supports caregivers in preparing for conversations that center safety, collaboration, and their child’s strengths.

Introduces trauma-informed care and explains how recognizing the impact of trauma helps create safe, supportive environments for children, families, and providers.

Explains how everyday sights, sounds, and experiences can unexpectedly trigger memories or emotions tied to trauma or loss. Helps caregivers understand these reminders and recognize how they may show up differently for each child.

Offers parents and caregivers a brief checklist to use to determine if a complete assessment for complex trauma should be scheduled. This fact sheet will help parents and caregivers determine when to seek professional help. Translated in 2025.
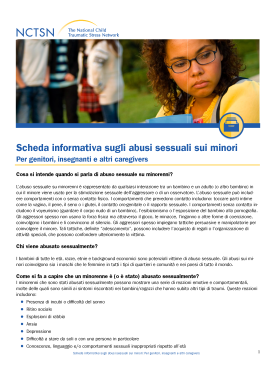
Defines and answers commonly-asked questions about child sexual abuse. This fact sheet outlines myths and facts about child sexual abuse and provides tips to help protect children. Translated in 2025.
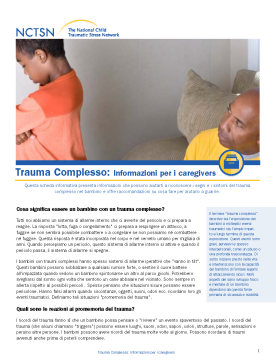
Helps parents and caregivers recognize the signs and symptoms of complex trauma and offers recommendations on how to help children heal. Translated in 2025.
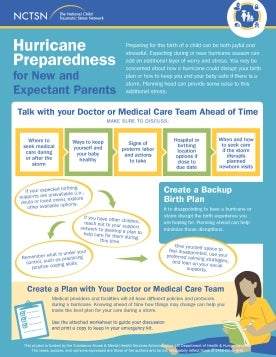
Helps new and expectant parents prepare for hurricanes by outlining practical steps to protect their health, baby, and birth plan. It includes planning tools, safety tips, and emotional coping strategies to reduce stress before, during, and after a storm.
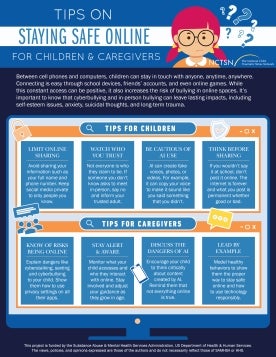
Offers practical tips for children and caregivers to stay safe online, recognize the risks of cyberbullying and AI misuse, and promote healthy, responsible digital habits.

Explores the complex relationship between bullying and trauma. Highlights how both targets and perpetrators can be affected by their environments and how these experiences shape emotional and behavioral responses.